Medicaid enrollment soared by 25% during the COVID-19 pandemic, but a big decline could happen soon
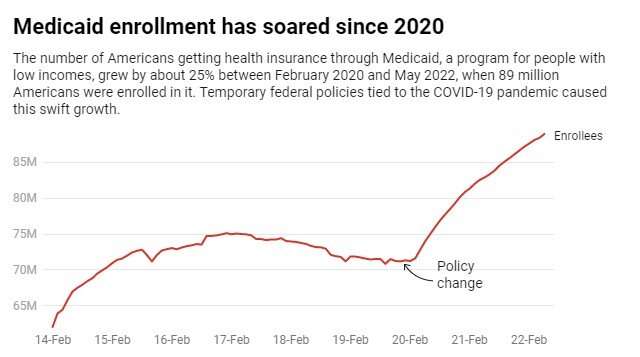
Medicaid, the government-funded U.S. health insurer for people with low incomes,grew by about 25%between February 2020 and May 2022 aspolicies adopted at the outset of the COVID-19 pandemicexpanded the program's reach.
All told, the number of people enrolled in Medicaid and theChildren's Health Insurance Program, or CHIP, which serves kids in families with low to moderate incomes,increased from 71 million to 89 million. That's roughly 27% of all Americans.
The pandemic-related increase in Medicaid enrollment was slightly larger than the24.7% increase seen after the Affordable Care Act(ACA) expanded Medicaid for adults, starting in 2014.
But unlike Medicaid expansion under the ACA, these pandemic policies are temporary. They will end once the federal government's COVID-19 public health emergency expires. Some experts predict Medicaid enrollment could fall by as many as15 millionpeople when this happens,disrupting health carefor many Americans.
In a new article we published in theJournal of the American Medical Associationon Sept. 20, 2022, we examine how Medicaid serves Americans, analyze the program's importance for health equity, and assess how Medicaid grew and changed during the COVID-19 pandemic.
Ashealth policyresearchers, we believe that Medicaid's growth since 2020 highlights the program's importance during economic and public health crises. It also underscores how painful the unwinding of these pandemic policies is likely to be to those who may end up uninsured.
Federal changes
In March 2020, Congress passed the first of several large spending packages, called the Families First Coronavirus Response Act. To help states shoulder increased Medicaid costs associated with the pandemic, that measure increased the share of Medicaid spending the federal government pays for by 6.2 percentage points in all states.
This aid has made a big difference for states, which分裂与联邦政府医疗补助计划的成本nment. Before the pandemic, the federal government was paying about 65% of Medicaid's costs overall, with the precise share varying based on a state's average income. States picked up the other 35% of Medicaid costs. These costs accounted formore than one-fourthof state budgets before the pandemic.
The extra federal money for Medicaid came with an important requirement: states accepting fundscould not remove anyone from Medicaidwho was enrolled as of March 2020 or gained Medicaid afterwards—as long as the official public health emergency,first declared on Jan. 31, 2020, remained in effect. Thesepolicies also applied to CHIP.
All 50 states and the District of Columbiaaccepted the higher federal payments in exchange for keeping Medicaid enrollment stable during the pandemic.
Greater stability
These changes helped to address longstanding instability in Medicaid coverage for many people. Before the pandemic,nearly 25%of those with Medicaid would enter or exit the program each year as their short-term circumstances changed.
People would lose Medicaid coveragewhen their income ticked up, their family circumstances changed, they aged out of CHIP, or they failed to complete required paperwork. Losing Medicaid coverage can lead to someone ending upwithout any health insuranceat all, which increases the likelihood they will postpone or never get needed care. Having the same people frequently entering and exiting the program also increases the program's administrative costs over time.
Changes to Medicaid policy in response to the pandemic made it much easier for everyone enrolled in Medicaid to keep their coverage. To illustrate, just over half of Wisconsin's Medicaid growth in 2020 came from that statekeeping existing enrollees in the programwho might otherwise have lost coverage for at least a few months.
Young adults, especially thoseaged 18 and 19, and Americans whorecently gave birthare two groups that benefited from this change in Medicaid policy.
What's next
Even with many aspects of daily life getting back to normal, andPresident Joe Biden's comments to the mediaabout thepandemicbeing "over," the official public health emergency that spurred Medicaid enrollment growth still remains in force.
When thegovernment renewed the declaration for the 10th timein July 2022, it set anew expiration date of Oct. 13, 2022. The administration also said it would provide states with 60 days notice before it would end the federal emergency declaration, which suggests the declaration will be renewed at least one more time.
When the emergency ends, states will have to reevaluate eligibility for everyone with Medicaid within12 months. Extra federal funding for states will also end.
These changes will have profound consequences. Millions of people will have to reestablish their eligibility for Medicaid and are at risk of losing coverage if they do not complete the required paperwork on time.
政府可能最终决定更新the COVID-19 emergency declaration again, ashundreds of Americans are still dyingdaily from the disease. Keeping it in place would prevent a massive drop in Medicaid enrollment and make it easier to continue other COVID-19 public health policies, such as makingfree COVID-19 testing and vaccinationswidely available.
Beyond extending thepublic health emergency, we believe that states and thefederal governmentcan seek new ways tominimize disruptionsin coverage and to make Medicaidmore accessibleto the millions of Americans who depend on it for health insurance.
This article is republished fromThe Conversationunder a Creative Commons license. Read theoriginal article.![]()



















