前列腺肿瘤生物学可能受生物学方面的影响c ancestry
Certain genetic variants found in prostate tumors of men of African descent were associated with African ancestry, according to two studies presented at the 15th AACR Conference on the Science of Cancer Health Disparities in Racial and Ethnic Minorities and the Medically Underserved, held September 16–19.
One of the studies was published concurrently in the journalCancer Research Communications.
In the United States, Black men have the highest rate ofprostate cancer-related mortality. Most studies examining disparities focus on race, which is typically self-reported and defined by skin color and social and cultural traits, explained Clayton Yates, Ph.D., the senior author on both studies, the director of the Center for Biomedical Research at Tuskegee University, and chair of the AACR Minorities in Cancer Research Council.
However, Yates argued, addressing health disparities will also require understanding the contributions of geneticancestrytotumor biology. Insights into genetic ancestry could aid precision medicine efforts by uncovering potential therapeutic targets specific to patients with African ancestry, he explained.
In the first study, Isra Elhussin, MBBS, MSc, a graduate student in Yates's research lab and an AACR NextGen Star, and colleagues examined the impact of African ancestry on the expression of immune inflammation gene signatures that are associated with higher immunogenicity and aggressive prostate cancers in men of African descent.
Elhussin and colleagues previously reported that prostate tumors from African American men had a two-fold greater activation of inflammatory signaling, which may contribute to the more aggressive disease typically observed in these patients.
However, Elhussin noted that the higher prostate cancer-related mortality among men of African descent is not limited to those living in the United States. "Men of African descent experience the highest rates of prostate cancer-related death around the world, suggesting a possible ancestral basis for these disparate outcomes," she said.
To determine the role of African ancestry in prostate cancer, Elhussin and colleagues sequenced prostate tumors from 72 patients in the United States who had not undergone treatment for their cancer. Among these patients, 16 self-reported their race as African American, 25 as European American, one as Asian, and 30 did not report a race. Using reference databases, Elhussin determined that most of the patients who identified as African American had genetic markers consistent with men of African descent, specifically those of the Bantu subpopulation (sub-Saharan) and/or the Yoruba subpopulation (Nigerian).
Compared with the tumors of patients with European ancestry, the tumors of patients with African ancestry were more likely to harbor mutations in SPOP, atumor suppressor genethat is mutated in approximately 10–15% of all prostate cancers. SPOP mutation has been previously linked to aggressive prostate cancer, Elhussin noted. Moreover, Elhussin found that SPOP mutation in patients with African ancestry correlated with increased expression of a pro-inflammatory immune gene signature, increased infiltration of immune cells into the tumor, and greater expression of the PD-L1 and PD-1 immune checkpoint proteins.
"We are the first to demonstrate that African genetic ancestry is associated with SPOP mutation, which leads to higher immunogenicity, upregulation of an immune inflammation signature, and higher tumor infiltration of immune cells expressing exhaustion markers, providing a potential mechanism for the higher prostate cancer-related mortality among men with African ancestry," said Elhussin. "These findings have implications for treating prostate cancers and could lead to new therapeutic strategies using anti-inflammatory drugs and immune modulators to decrease the disease burden among men of African descent."
"While most prostate tumors do not have immune cell infiltration, our findings show that prostate tumors with this SPOP mutation have very high levels of immune cell infiltration," noted Yates. "This is an exciting discovery that may help identify patients who would benefit from immunotherapy, which is particularly important given that African Americans are often underrepresented in clinical trials evaluating such therapies."
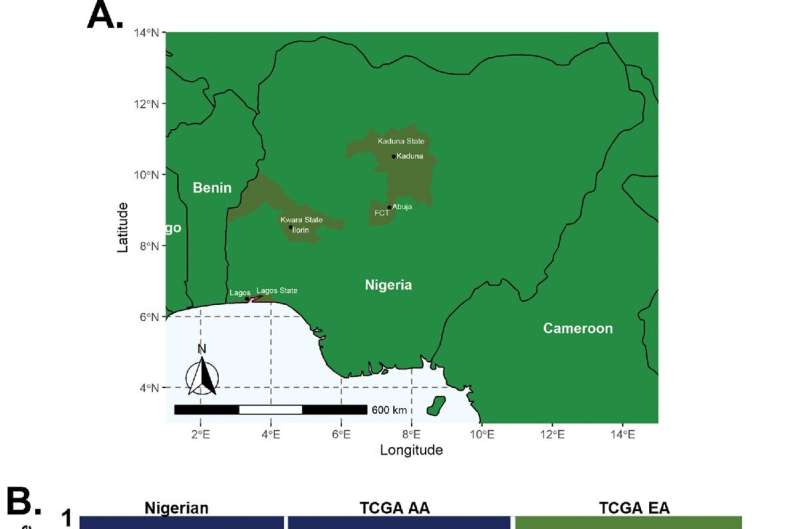
In the second study, which was concurrently published inCancer Research Communications, Yates and colleagues, including first author Jason White, MS, compared DNA sequences from prostate tumors of Nigerian, African American, and European American patients. The study was completed in collaboration with the Prostate Cancer Transatlantic Consortium (CaPTC).
"Our goal was to understand the genomic contributions to prostate cancer among Nigerian men, something that had never been studied before," said Yates. "We performed sequencing to determine if there were unique mutations associated with the Nigerian population that were distinct from those in tumors from African Americans or European Americans, as well as to identify any similarities across these populations."
Yates, White, and colleagues sequenced 45 advanced-stage treatment-naïve prostate tumors and 11 unmatched non-tumor prostate samples collected from Nigerian patients. They compared these sequences with existing data from African American and European American prostate tumors in The Cancer Genome Atlas database.
They found that genetic variants were similar between the Nigerian and African American prostate tumors, with specific variants in the BRCA1 DNA repair gene among the most frequent variants identified in both populations. Furthermore, the researchers determined that the frequency of BRCA1 mutations increased with higher proportions of African genetic ancestry and decreased with lower proportions of African ancestry.
"We identified unique variants in the BRCA1 gene that are not typically tested for in the clinic, and these variants were specific to African ancestry," said Yates. "On the other hand, tumors from European Americans had variants in different DNA repair genes that were not observed in tumors from African American or Nigerian patients. This suggests that different variants contribute to prostate cancer in European Americans compared with men with African ancestry."
These findings may have implications for the treatment of prostate cancer in patients of African descent, Yates explained. "The BRCA variants currently tested for in cancer were identified from a non-minority population and do not include the variants specific to African ancestry that we identified," he said, adding that this effectively excludes many African Americans from BRCA-targeted cancer therapies.
"Testing for these additional variants would help identify additional patients eligible for BRCA-targeted therapies and may provide some prognostic value as well," he added. Future studies will aim to understand how the identified variants contribute to prostate cancer development and progression, Yates noted.
Together, these studies highlight the contributions of African ancestry to prostate cancer genetics and may explain some of the racial/ethnic disparities in outcomes among patients with prostate cancer, explained White, who presented the research on Nigerianprostate tumorsat the AACR Disparities Meeting. He added that epigenetic and societal factors are also important contributors to cancer health disparities.
Limitations to both studies included small sample sizes, a scarcity of biospecimens from racial/ethnic minorities, and underrepresentation of Africans in genomic studies and in existing databases, Elhussin noted.


















