Telehealth brings big advantages for older adults, but new 'guard rails' could significantly bolster care
Today's telemedicine providers are only scratching the surface of what's possible in providing high-quality health care to people who need it most—and especially to older adults who benefit greatly from its accessibility, according to researchers and clinical experts from West Health.
The solution, they say, is for telemedicine providers to set the bar higher by following guidelines that ensure remote care is delivered in the best way possible to seniors.
"The COVID-19 pandemic brought to light the immense value of telemedicine to remotely connect patients and doctors for a wide range of health care needs," says Liane Wardlow, Ph.D., senior director of Clinical Research and Telehealth at West Health. "But when treatingolder patients, we see that telemedicine falls short in many important ways. The problem is that remote health care delivery simply wasn't designed with the needs of older people in mind."
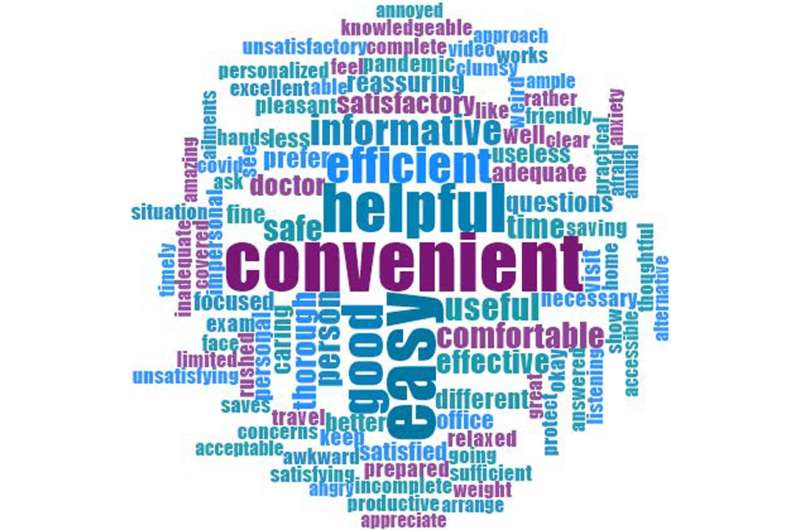
In an editorial published in the latest issue of theJournal of the American Geriatrics Society, Wardlow and West Health's Chief Medical Officer Zia Agha, M.D.—along with their collaborators from University of North Carolina and University of Pittsburgh—offer commentary around a new peer-reviewed report showing that people who are 65 and older appreciate telemedicine's convenience and want it to remain available but have had frustratingtechnical challenges等问题,阻碍了他们的经验。
"The pandemic has taught us that our health care system is vulnerable and needs to adopt capabilities liketelehealthin order to deliver safe and effective care in the future," the authors write.
To solve the problems that are holding back telemedicine, they argue a framework is needed to ensure providers can offer care that meets three key requirements.
First, telehealth must be person-centered to enable visits where patients feel connected and heard. It also must be equitable and accessible to people of all backgrounds, as well as to those with possible cognitive impairment and those living in areas where quick Internet access isn't a given. Finally, telemedicine must be integrated and coordinated with patients' overall care plans; providers should also understand the patient's social support structure and ability to obtain prescribed medications.
"Without these guard rails, telehealth may further segment care, thereby increasing the chances of low-value care while further exacerbating health inequities," the authors write. "With these guardrails in place, however, telehealth has the potential to realize its promise of improving access to high-value, equitable, safe, timely and convenient care to older adults."
In addition, they say it's imperative that providers are trained in skills unique to offering remote care toolder adults: "Simply because a provider is well-trained in supplying in-person care does not mean that the same provider is capable of providing high quality care using telehealth," they say.
The authors are among key drivers in the creation of a national Center of Excellence for Telehealth and Aging, which is developing first-ever industry guidelines for age-inclusive telehealth.
米ore information:Kevin Biese et al, Telehealth with older adults: Getting it right,Journal of the American Geriatrics Society(2022)。DOI: 10.1111/jgs.18090
Roma Bhatia et al, Older adults' perspectives on primary care telemedicine during the COVID ‐19 pandemic,Journal of the American Geriatrics Society(2022)。DOI: 10.1111/jgs.18035




















