This article has been reviewed according to Science X'seditorial processandpolicies.Editorshave highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Study unravels a cause of resistance to novel drug in patients with acute leukemia
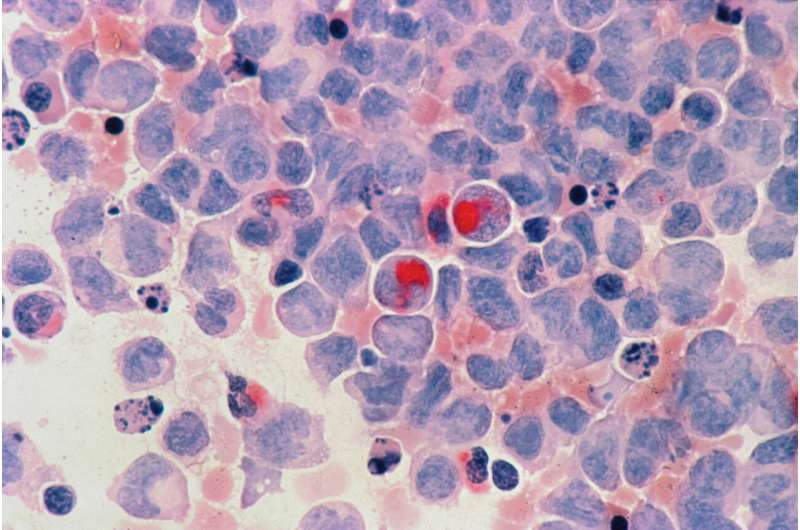
A new targeted drug has not only sparked remissions in patients with a common form of leukemia but also induced the cancer cells to reveal one of their schemes for resisting the drug, investigators at Dana-Farber Cancer Institute and other research centers report in a new pair of studies in the journalNature.
One of the papers presents results of a clinical trial in which approximately 40% ofpatientswith acute leukemia subtypes had a complete response—a disappearance of all signs of cancer—to treatment with thedrugrevumenib. The other paper uncovers a molecular countermove by whichleukemia cellscome to sidestep the drug and reassert their growth.
The papers point to the promise of the targeted approach to acute leukemia treatment exemplified by revumenib and to the potential to extend its benefits with drugs that trip up the resistance mechanism, researchers say.
"The two genetic subtypes of acute leukemia involved in this research account for approximately 40% of all cases of acute myeloid leukemia (AML) in children and adults," says Scott Armstrong, MD, Ph.D., president of the Dana-Farber/Boston Children's Cancer and Blood Disorders Center and co-senior author of the paper on revumenib resistance. "They're driven by a rearrangement of the MLL1 gene or a mutation in the NPM1 gene. Both types depend on a protein called menin to sustain their growth."
The first of the newNaturestudies reports on a phase I/II clinical trial of the drug revumenib, which targets menin, in 68 patients with acute leukemia that wasn't responding other therapies. The trial, dubbed the AUGMENT-101 study, found that of 60 patients who could be evaluated, 53% responded to the drug and 30% had a complete response.
"For patients with acute leukemia who have undergone several previous treatments, this is a very encouraging result," Armstrong says. "However, after the second cycle of treatment, some patients did develop resistance to revumenib."
In their follow-up study, Armstrong and his associates sought a source of that resistance.
Menin is a critical part of the cell's "epigenetic" mechanism for switching gene activity on and off. It binds to chromatin—the braid of DNA and protein packaging within the nucleus—and summons large protein complexes to join it. The complexes tighten or loosen the coils of DNA, changing the activity level of the genes at that site. One of the key proteins within these complexes is MLL1, the product of the MLL1 gene.
"Revumenib contains a small molecule that inhibits the interaction of menin and MLL1," Armstrong says. "The AUGMENT trial shows it can produce remissions in a high percentage of patients."
When Armstrong and his colleagues analyzed bone marrow samples from some of the patients who became resistant to revumenib, they found that many had developed mutations in MEN1, the gene that gives rise to the menin protein. The mutation leads to a deformed version of menin that doesn't bind well to revumenib but attaches as firmly as ever to MLL1. As menin and MLL1 renew their interaction, leukemia cell growth restarts.
The finding provides "formal proof in patients that menin itself is a valid target for therapy in both genetic subtypes of AML," Armstrong relates.
In a sense, revumenib acts as a kind of truth-telling serum on leukemia cells: by placing the cells under pressure, it prompts them to divulge one of their strategies for survival. "The fact that the cell has gone through so much trouble to mutate MEN1 in order to survive is a strong indication that we're hitting a target the cell truly relies on," Armstrong states.
The ability of revumenib to stress leukemia cells to the point where they develop a mutation to remain alive is testament to the drug's effectiveness, he continues. "This is the first time a drug targeting a chromatin-binding protein complex has been shown to put that degree of pressure on cancer in a human patient."
By tracking the development of mutations in MEN1 and other genes in patients with acuteleukemia, doctors may be able to identify patients at high risk of relapsing, Armstrong relates. Such patients might then benefit from further treatment. The discovery of MEN1 mutation as a resistance mechanism suggests that new drugs that specifically target menin or other chromatin-associated proteins could prevent or delay revumenib resistance or treat patients who have become resistant to the drug.
“看到tran阿姆斯特朗博士的工作slated elegantly into the clinic where patients—including some at Dana-Farber, who had dramatic responses in dire situations—was highly gratifying personally and professionally," says Dana-Farber's Richard Stone, MD, a co-author of bothNaturestudies. "We are now ready to magnify the impact of these results by conductingclinical trialscombining revumenib with standard chemotherapy as well as with novel agents, also based on preclinical work done in great part by Dr. Armstrong."
更多的信息:Richard Stone et al, MEN1 mutations mediate clinical resistance to Menin inhibition,Nature(2023).DOI: 10.1038/s41586-023-05755-9.www.nature.com/articles/s41586-023-05755-9
Ghayas Issa, The menin inhibitor revumenib in KMT2A-rearranged or NPM1-mutant leukaemia,Nature(2023).DOI: 10.1038/s41586-023-05812-3.www.nature.com/articles/s41586-023-05812-3




















